COVID19 in rural India: Shortage of PHC doctors, preference for quacks and high vaccine hesitancy
A recent rural survey of 300 respondents in Jhabua, Madhya Pradesh, found 38% respondents preferred quacks for treatment, commonly known as nadi babas. Against 14% registering for COVID vaccination, only 4% went ahead for inoculation. These challenges need to be addressed urgently as the virus has spread in rural India.

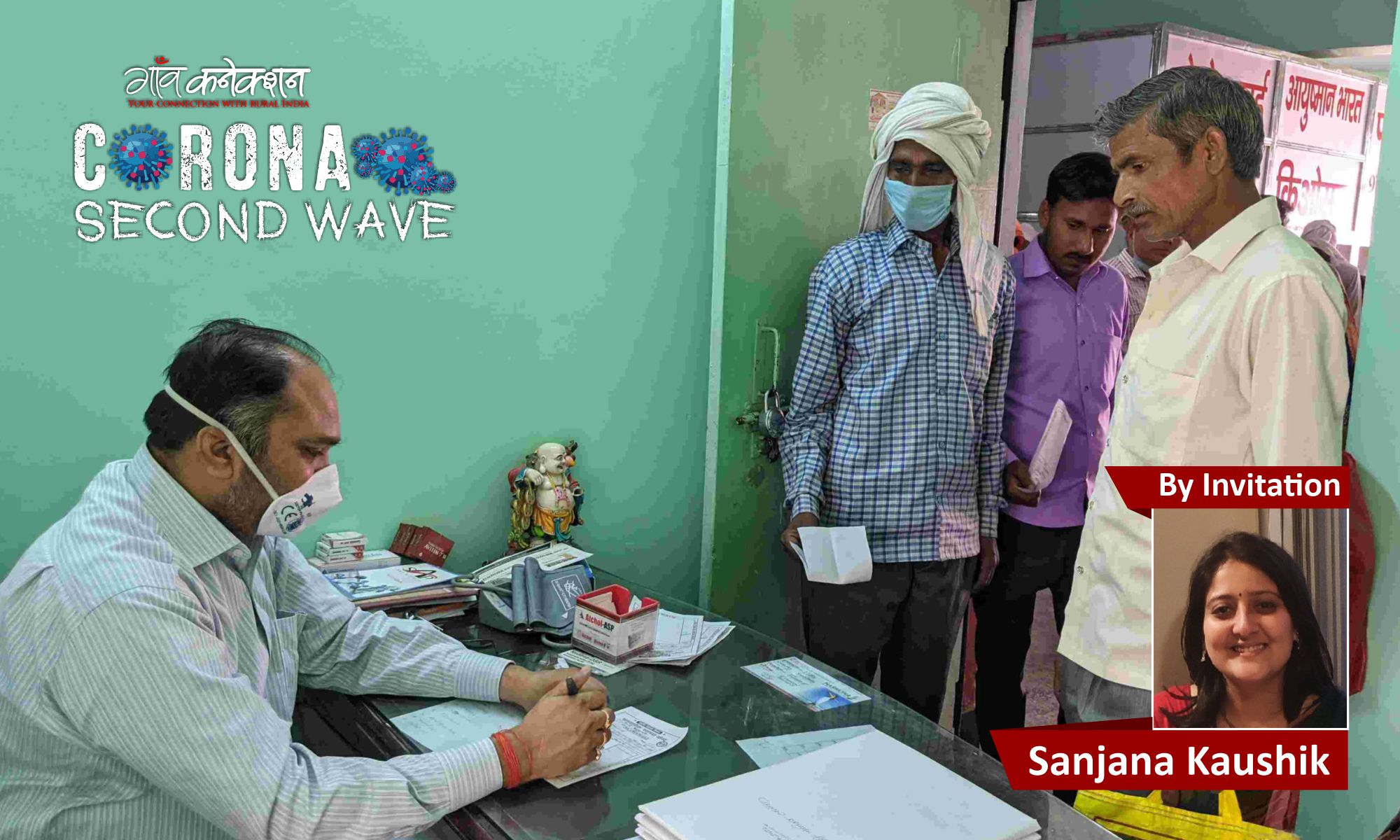
Data shows only 39 per cent of rural respondents prefer visiting government hospitals for their treatment. All photos: By arrangement
Sixty five per cent of India’s population resides in rural areas, while only 33 per cent of the health infrastructure caters to their needs. The rural healthcare infrastructure is three-tiered and includes a sub-centre, a Primary Health Centre (PHC) and a Community Health Centre (CHC). As per reports, these PHCs are short of over 3,000 doctors, with the shortage having increased by 200 per cent (or tripled) over the last 10 years.
Due to numerous reasons and the second COVID wave, there has been a spike of infections in rural India, which had been doing better until now. According to reports, cities like Delhi and Mumbai are in immense trouble – which is true – but they have neglected the dire situation of villages, where the lack of health workers, oxygen and proper facilities is nothing but frightening.
The rural community is scared and anguished. With the first wave gone, most forgot about the disease and moved on, especially in rural areas as its impact was not felt as much. But a couple of weeks ago, in Petlawad, a remote block of Jhabua district, Madhya Pradesh, as the second wave hit, almost every third villager started showing symptoms, and no one was prepared.
The health infrastructure was not only unprepared, but also ill-equipped to combat the virus. The few medical staff that are there, are hesitant to treat patients due to fear for their families and their own wellbeing. The second wave is destroying livelihoods and taking away loved ones from rural communities leaving them vulnerable.

Preference for quacks
People in rural India do not easily trust the treatment offered by allopathic doctors and advanced healthcare facilities, owing to cultural backwardness and anecdotal evidence. As many got infected, they chose to visit nadi babas or quacks for their treatment. Many even hid their symptoms from others, to avoid consulting doctors and facing the stigma that comes with the COVID-19.
To understand this distrust, Transform Rural India Foundation (TRIF), a multi-partner initiative, conducted a dipstick survey from May 4 to May 19 in Jhabua, Madhya Pradesh, with 300 respondents.
Also Read: There’s more to India’s COVID19 death toll than meets the eye
Data showed that 38 per cent of rural respondents prefer to go to quacks and nadi babas for their treatment. While 39 per cent of the population visits government hospitals. But, most of them choose to not get admitted. The rest (23 per cent) do not prefer to go to any of these and wish to get cured at home itself.

Vaccine hesitancy
The same survey also revealed some data on vaccination. While only 14 per cent registered themselves for vaccinations, a mere four per cent went ahead and got inoculated. This is the case in most Indian villages, which makes herd immunity a far-fetched idea.
But why do people not want to get vaccinated in the first place? Most of them associate vaccines – and allopathic drugs in general – with sudden and mysterious deaths. Despite numerous sessions, dissemination of information in regional languages, and Q&A sessions, the majority of village residents are unconvinced that vaccination could protect them from the virus.
There are rumours around the vaccines: People have associated some of the recent deaths in their areas to the vaccine rollout, while the reality is far from it. Some people died due to pre-existing conditions or not being eligible for vaccinations in the first place, (people with a complicated medical histories or comorbidities, weak immune systems, pregnant and lactating mothers, alcoholics) and were misinformed about the same. Most people did not consult a doctor before getting their shot and faced serious health consequences because of it.
Apart from this, there was a problem in the rollout itself. Vaccines could not be stored by the authorities at the right temperature as facilities to do so often do not exist in rural areas.
Also Read: Can Tamil Nadu’s robust public health system control the second wave?

Lack of testing, wrong treatment
While the survey was helpful in understanding people’s apprehensions about vaccinations and doctors, data also showed there was a disbelief around COVID19 deaths. Most of the deaths were attributed to typhoid and not COVID-19, as the villagers chose to visit quacks, who told them they had typhoid. These patients took medicines too but refused to go for an RT-PCR test.
Some of them recovered as their infection was not severe enough. But many of them did not survive as they were not given proper treatment and care. The disease was never detected as they refused to get tested, and as a result, deaths could not be counted accurately.
What can be done?
It is important to keep the dialogue with rural communities alive and provide them with the right information. To be able to do so, grassroot level organisations need resources to be able to help vulnerable communities.
It is important for frontline workers, both medical and social workers, to feel supported and acknowledged. A healthy discourse on rural communities in the media will go a long way.
Organisations working in the grassroots are also adapting to the health crisis. For instance, TRIF reached out to tribal leaders in an attempt to educate the populations and positively influence individuals from within their community.

Above all, it is important to reassure them to get proper medical treatment. The government, as well as non-profits, should support them to provide necessary equipment and resources and assure them that they will not be left alone in this apocalypse.
For people living in urban spaces, an acknowledgement of the problem is the first step. It is imperative to learn about India’s rural spaces, where only one allopathic doctor is available for every 10,000 people. Educating others is important too.
Lastly, if you can, support organisations that are tirelessly working to serve these communities.
Sanjana Kaushik is a Block Engagements Manager at Transform Rural India Foundation. She works closely with communities in the tribal belts of Jhabua, Madhya Pradesh and anchors the Block Transformation Program. You can read about TRIF’s contribution here.

