WHO’s approval of malaria vaccine brings cheer to malaria saathis and doots in tribal Koraput district of Odisha
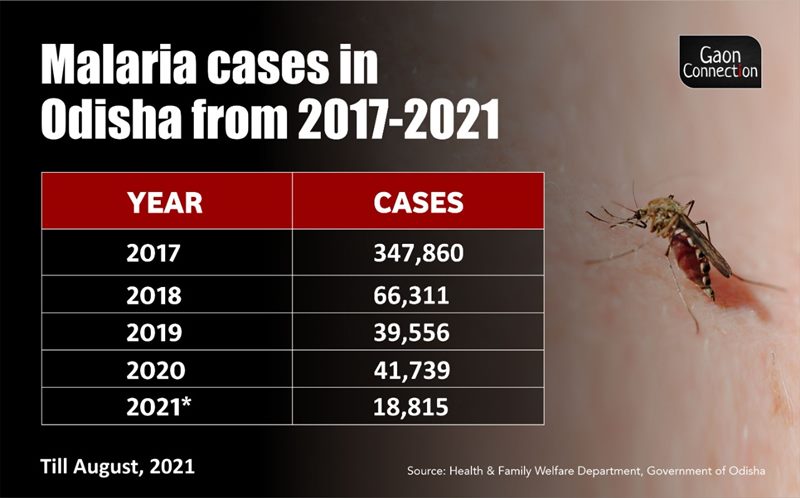
Odisha has been successfully using a community-driven programme comprising malaria saathis and doots, who work with the ASHA workers and ANMs, to spread awareness on malaria prevention, conduct rapid testing and quickly distribute medicines. From 2017 to 2020, malaria incidence has come down from 347,860 to 41,739 in the eastern state which plans to eradicate the vector-borne disease by 2030. A ground report from the malaria endemic Koraput district.
Chintaguda (Koraput), Odisha
Tulsi Habika cannot thank her local malaria saathi enough. A member of the Dongria clan of the Kondha tribe, the 40-year-old resident of Khajaguda village had a harrowing time in September when her six-year-old son Rajiba “writhed in pain, vomited a lot and had a fever”.
“I informed our saathi Rajendro and he tested my son and gave some medicines. Thereafter, we took my son to the hospital in Narayanapatna where a doctor applied sui and botal (administered injection and saline) and advised us to continue the medication,” said Tulsi, who was grateful to the saathi and the doctor for timely help that saved her six-year-old’s life who had tested malaria positive.
The tribal village Khajaguda is in the Narayanpatna block of Koraput district, about 500 kms from the state capital Bhubaneswar. Koraput has a significantly high Adivasi population living in remote hamlets located amidst hills and dense forests. Malaria is endemic in this region and Koraput has a high incidence of this vector-borne disease. The district is often in the news for Naxalite insurgency.

The recent approval of the world’s first malaria vaccine on October 6, by the World Health Organization (WHO), has brought both hope and cheer to the local community health workers, such as malaria saathi Rajendro in Koraput, who are the backbone of the state’s programme to eliminate the disease by 2030. The new vaccine has rightly created a buzz amongst the state health officials in Bhubaneswar.
“So far, the malaria vaccine has been used in Ghana, Kenya and Malawi in Africa. The central government will hopefully procure it and we believe that it will help reducing the malaria incidence, especially in children,” Shubhashisha Mohanty, who is based in Bhubaneswar and is Odisha’s state programme officer of the National Vector Borne Disease Control Programme (NVBDCP), told Gaon Connection.
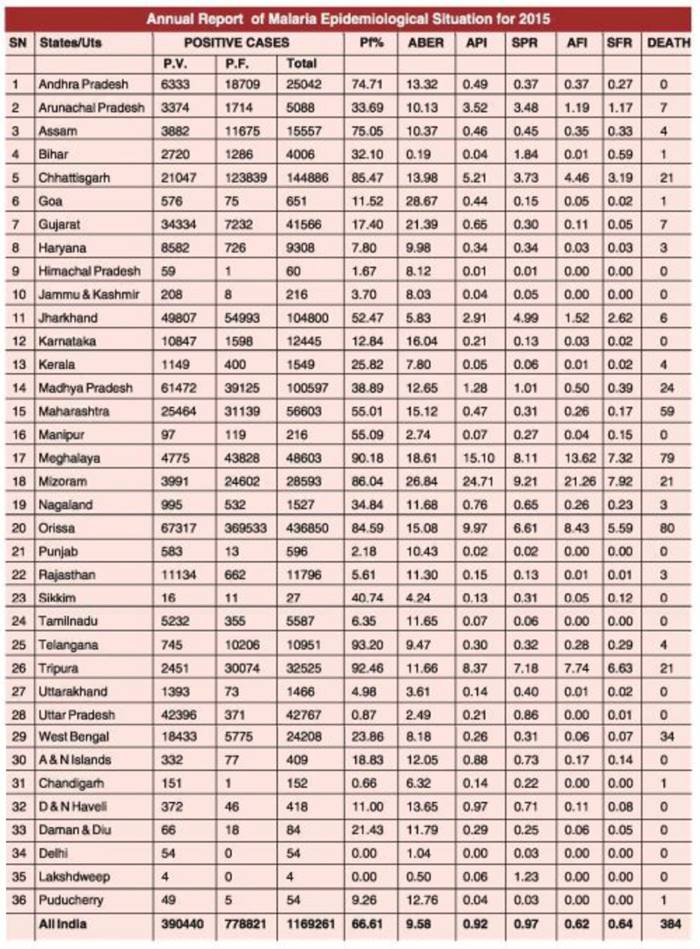
As per this national programme’s official data, Odisha’s malaria caseload has traditionally been the highest in the country.
Also, according to a press release issued by the Press Information Bureau on December 2, 2020, states of Odisha, Chhattisgarh, Jharkhand, Meghalaya and Madhya Pradesh disproportionately accounted for nearly 45.47 percent (1,53,909 cases out of India’s 3,38,494 cases) of malaria cases in India.
A grassroots operation to eliminate malaria
The Odisha government is running a grassroots programme to control and eliminate malaria in the state. In August 2018, it entered into a memorandum of understanding (MoU) with Malaria No More, a New York-based non-profit organisation, and launched a joint initiative. The non-profit works along with the state government healthcare department in Bandhugaon, Boipariguda and Narayanpatna blocks of Koraput, known for their high prevalence of malaria. As per Niranjan Mishra, Odisha’s director of public health, more than half of the malaria cases in the state are reported from the southern districts of Koraput and Malkangiri.

Also Read: Zika virus cases soar to 105 in Kanpur; CM Yogi Adityanath assures no need to panic
“Koraput is full of hilly and forest areas. There are 776 villages that are hard to access and are home to tribal inhabitants whose scant clothing also makes them vulnerable to mosquito-bites. Reaching healthcare services to areas that aren’t connected to motorable roads is a challenge,” Makaranda Beura, Koraput’s chief district medical and public health officer, told Gaon Connection.
The malaria control initiative utilises a model based on local community participation and saathis (meaning companion) are the fundamental unit of this programme.
“Our functioning is such that we employ people from the local community and train them to spread awareness, supply medicines, conduct rapid antigen tests and maintain registers on the malaria situation in their area of operation,” Santosh Kumar Baghar, Malaria No More’s district programme manager in Koraput, told Gaon Connection.

According to Baghar, there are three levels of community representatives on the ground — malaria saathi (companion), malaria doot (messenger), and the field supervisor.
The community-driven malaria elimination programme is also empowering many rural women who have been appointed as saathi in their villages. These women not only raise awareness about malaria in the hinterland but also collect blood test samples from suspect patients for malaria and distribute medicines. For a person to be appointed as a saathi, she or he needs to be literate in the Odia language. There are 60 saathis and 18 malaria doots in the Koraput district.

About 24 kms from Narayanpatna community health centre (CHC), 21-year-old Mita Tadingi is a malaria saathi in her village, Chintaguda.
Also Read: Rural Bihar in the grip of ‘viral fever’; children suffer the most, paediatric wards full
“I was trained by MNM in July, last year, to conduct blood tests, survey households, and spread awareness amongst the villagers. The villagers respect my work and I earn almost three to four thousand rupees a month,” Tadingi told Gaon Connection. “The CHC has now appointed me as an ASHA worker,” she added.
The Patient-Saathi-Doot-ANM partnership
As part of the grassroots programme to eliminate malaria, there is a strong partnership between the villagers, malaria saathi, malaria doots and the government-appointed auxiliary nurse-midwives (ANMs).
“The saathis are usually young people who can read and write Odia. They ensure that preventive measures are taken by the villagers and test suspected cases of malaria,” explained district programme manager Baghar. “If a patient tests positive for malaria, the saathi approaches the malaria doot who in turn contacts the nearest sub-centres for medicines that are given to the patients through the saathis,” he explained.

A saathi looks after a single village or a hamlet while a doot is responsible for supplying medicines to three to five such villages. The malaria doots works parallelly with the government-appointed ANMs. The saathis also use a rapid diagnostic test (RDT) for diagnosing the patients with malaria. Its results arrive within 20 minutes and it is conducted in the village itself.
The field supervisor works at the block level and is responsible for physically collecting the data of malaria cases each month and bring it to the District Project Management Unit at Koraput.
“We assign the field supervisor role to youngsters who have a bike as the distance between villages and to our office can be as much as 100 kilometres,” said Baghar.

“Ours is a Maoist-affected district. We are often stopped by the Maoists for identification but they do not bother us once they learn that we are working for the health of the poor, tribal villagers,” Gotapu Sagar, Kumar, a field supervisor from Bandhugaon block, told Gaon Connection.
Working in the Naxalite-affected district has not been without its challenges.
Explained: What is the D2 variant of dengue that has wreaked havoc in Uttar Pradesh’s Firozabad
“The term we had proposed initially was malaria soochak which in Hindi translates as ‘malaria informer’ but the word ‘informer’ can get one into trouble in a district that is battling insurgency,” Biswajeet Mohapatra, Malaria No More’s state-in-charge shared with Gaon Connection. “The officials advised us to change it to something more friendly. We decided on saathi which means a companion,” he added.
Focus on preventive measures for malaria control
“Ensuring behavioural changes to eradicate malaria can only be possible if the community is involved. The appointing agents of change should be from within the community. We greatly appreciate the role of ASHAs and the malaria saathis for this,” Susanta Kumara Das, additional director of the vector-borne disease control wing of the health department in Koraput, told Gaon Connection.
“It is participation of the local community in government initiatives that make them successful. Mass screening, vigilant reporting of cases, convincing the tribal population to wear suitable clothing, promoting the use of long lasting insecticidal nets after sunset, and ensuring patients follow treatment protocol is only possible due to the involvement of the community,” the additional director added.
Long lasting insecticidal nets, indoor residual spray and the DAMaN (Durgama Anchalare Malaria Nirakaran) initiative (malaria control in inaccessible areas) have proved to be significantly effective in controlling the disease.

Insecticidal mosquito nets are coated with chemicals and are effective for a period of three years. They have to be changed every three years. “The Union government has provided these nets to Odisha and, we are hopeful of making Odisha malaria-free by 2030,” the additional director said.
Das also emphasised that it was extremely important to ensure that the patient receives the full treatment because otherwise the gametocyte in the patient’s blood could enable more mosquitoes to become the carriers of malaria and the situation could worsen in no time.
School children are also being educated about malaria through interactive charts and awareness programs, Das said.
Also Read: Battered by floods, Varanasi now hit by dengue outbreak
Adding to this, Niranjan Mishra, director of state’s health and family welfare department in Bhubaneswar said that increase in literacy, better road connectivity and improved healthcare facilities had decreased the prevalence of malaria in the state.
Hello Points at distant villages
One of the major challenges in executing the measures to control the incidence of malaria is connectivity, said Santosh Kumar Behera who is the technical support supervisor at the community health centre at Koraput’s Narayanpatna block.
“I have to send timely data every month to the district headquarters so that they can assess the malaria situation. But due to the disruption of mobile connectivity and the internet, we are delayed in sending the reports,” he said.

In order to optimise connectivity in the far flung areas, the doots have identified locations where the mobile connectivity is not too bad. “We have named such areas as ‘hello points’ which are used for communication from the remote areas on the hills,” Biswajit Mohanty, told Gaon Connection.
Some malaria saathis and doots also pointed out the lack of medicine supplies at times.
“Sometimes just getting the medicines from the ANM and the subcentres can take more than a day and we can’t reach the medicines to the patients on time,” Nagesh Huika, a 20-year-old malaria doot, told Gaon Connection as he picked up the medical supplies from the Jogipalur sub-centre.
Another hurdle is the discrepancies that creep into the record keeping of the malarial cases.

“Sometimes there is a mismatch in the government report and the MNM report. It suggests that villagers are bypassing malaria saathis and are directly coming to the government health centres to report their cases. This results in fewer cases being documented by the non-profit than the actual count,” observed Susanta Kumar Das, additional director of the vector-borne disease control wing.
These minor roadblocks aside, both the state machinery and the grassroots workers seem confident about eradicating malaria by 2030 from India’s one of the worst affected states. And the recent approval of the malaria vaccine only strengthens their resolve.

