Leaking roofs, missing doors, weeds everywhere and few staff: Rural health centres in shambles
A primary health centre is the first step to access basic healthcare facilities in rural India. In the second wave of the pandemic that has hit villages, the importance of these centres has multiplied manifold. But, a number of these centres are dilapidated and non-functional, reveals a Gaon Connection report from rural Uttar Pradesh.

Standing outside the locked rusty grill gate of his village’s primary health centre (PHC), 43-year-old Kallu Verma, a resident of Pasa Khera village in Uttar Pradesh’s Unnao district, nonchalantly said that the centre has had no doctor for the past three months.
“If we need a doctor, we visit Purwa block’s CHC [community health centre] which is 12 kilometres away. If better medical attention is needed, we prefer to go to Unnao which is 35 kilometres away,” Verma told Gaon Connection.
“The health centre is opened once in a week or fifteen days, but only for teekakaran (regular immunisation) and then shut down,” he added.

As the second wave of COVID19 sweeps across rural India with village after village reporting corona cases, yesterday on May 28, community journalists of Gaon Connection visited 11 rural health centres — four PHCs and seven sub-centres (upkendras) — in the villages of Unnao, Barabanki, Shahjahanpur and Sitapur districts.
Also Read: With no tests and no treatment, people in rural India are dying of COVID-like symptoms
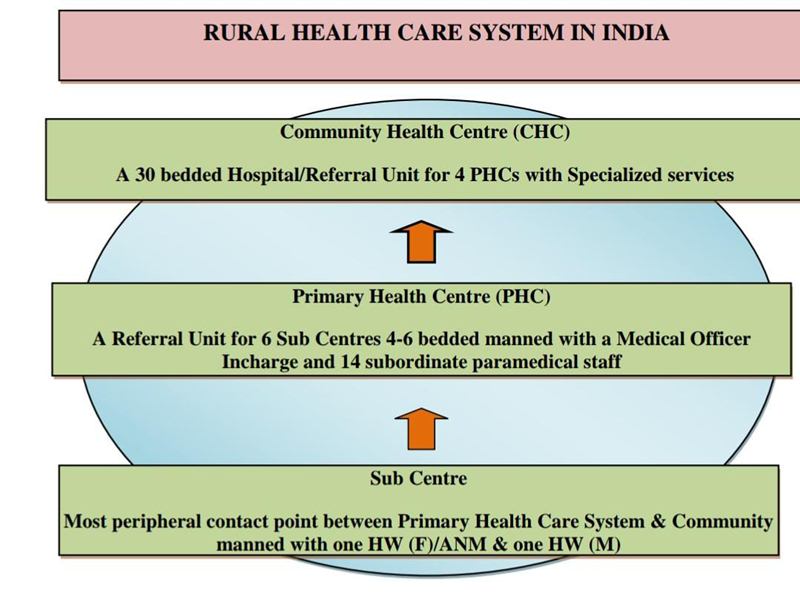
These health centres are exceedingly vital for India’s villages as these are the fundamental units of rural health infrastructure where villagers access basic medical facilities, at least on paper.
However, Gaon Connection found that several of these primary health centres were in dilapidated and deserted conditions. Some had their doors, windows and scanty furniture broken with no staff in sight. Some were locked with overgrown weeds.
With cow dung stored inside some of them, garbage heaps adding to the unhygienic conditions, and goats grazing around the premises, these health centres showed clear signs of neglect and abandonment.

Sub-human conditions to work in
Almost 180 kilometres from the Pasa Khera’s PHC, the situation was worse in Shahjahanpur district’s Khairpur village as the sub-center was found to be in a dilapidated condition and seemed on the verge of a collapse.
The lavatory inside the health center was found to be locked and the hygienic conditions were in shambles.

“There’s nothing here. It has no gate or doors, the room’s ceiling leaks when it rains, we ASHA workers get drenched while working inside it. The structure is so fragile and damaged by water that it can possibly collapse some day,” Nirmala Devi, an ASHA (Accredited Social Health Activist) worker in Khairpur, told Gaon Connection.
“Kisi din mar jayenge dab kay isme [one day we will bury under it and die],” said Devi as her voice broke in a fit of anger and helplessness.

“It’s a sub-human condition to work in. I wonder why the washrooms of the centre are locked. Due to the absence of doors and gates, we women feel insecure while working here,” Devi added.
Also Read: COVID-19 invades rural India; district hospitals struggle with faulty or no ventilators at all
While talking to Gaon Connection, an elderly lady of Khairpur village expressed her angst. “I have been seeing this centre for about twenty years now. Nobody cares about it. It is not fit for anybody to work in,” Sudama Devi said.
Meanwhile, about a hundred kilometres away from Khairpur, the primary health centre in Belahra village in Barabanki district’s Fatehpur block wore a ‘new look’. The local people told Gaon Connection that the centre had been repaired about six months ago.
“Before Corona, 50-60 patients used to come here on a daily basis. But now they are afraid that if they visit the centre, they will be tested for COVID. Today only three people have visited the centre for a check up,” a health official told Gaon Connection on the condition of anonymity.

Not very far from the PHC of Belhara, the residential quarter of the medical staff was found to be in a mess with no sanitation or arrangements for the doctors to live in it.
Also Read: “I have to wait for nine months to be paid Rs 600 incentive for one delivery”
In Barabanki’s Chheda village in Suratganj block, the PHC centre was found to have no arrangement for water supply and is located amidst heaps of garbage around it.
PHCs without doctors
According to a 2018-19 report released by the Union Ministry of Health and Family Welfare, as per the official norms, an average of 35,567 rural residents depend on a single PHC in the country. For sub-centers, each unit covers, on an average, a population of 5,616. The numbers are expected to be much higher for Uttar Pradesh, India’s most populous state with a population of over 200 million.

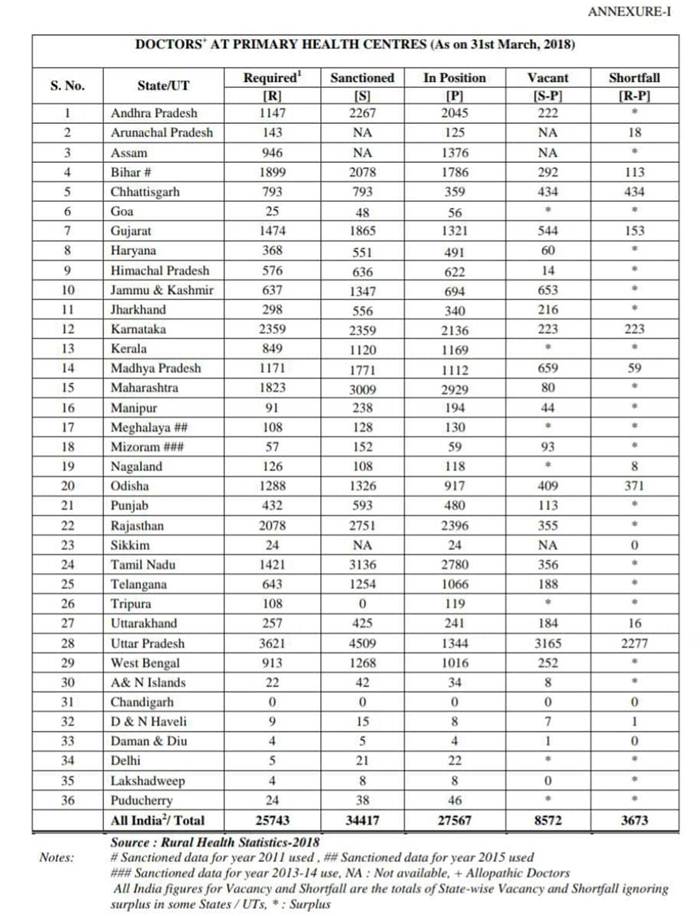
According to a reply submitted by the Union Health Ministry in the Lok Sabha on November 22, 2019, the PHCs in Uttar Pradesh (UP) have one of the worst doctor to patient ratios in the country.
The reply showcased that Uttar Pradesh has a sanctioned strength of 4,509 doctors for PHCs but has a total number of 1,344 doctors with 3,165 seats being vacant, exhibiting a deficit of 2,277 doctors.
On April 1 this year, amid the raging second wave of the pandemic, Amit Mohan Prasad, Additional Health Secretary to the UP government, had informed that half of the total COVID19 cases in the state were being reported from its rural areas.
“The situation has worsened ever since the COVID19 pandemic has invaded rural areas in the state and health workers in charge of these health centres are doubling up for their Corona-related duties,” Madhu Garola, chief medical officer (CMO), Sitapur district, told Gaon Connection.
Understaffed PHCs
According to the Indian government’s guidelines, mentioned in the Union Health Ministry’s Rural Health Statistics report for 2018-19, the minimum norm of staffing pattern requires a sub-center to have at least three health workers — a female health worker/auxiliary nurse-midwife (ANM), an additional ANM on contractual basis, and a voluntary worker.
The same guidelines specify that a PHC should have a minimum of 15 staff strength including four medical officers, seven nurse midwife, ward boys, pharmacist/compounder, laboratory technician, etc.

However, the ground reality is far from what is mentioned in these official guidelines.
In Sitapur district’s Pisawan village in the Jalalnagar block, an incharge pharmacist at the sub-center told Gaon Connection that there the centre was equipped with two male health workers only — a wardboy and himself.
“For the last one-and-a-half-year, ever since the COVID19 began, I have been tasked with the RRT (rapid response team) so I am not in a position to look after the sub-center daily,” Arun Kumar Rastogi, incharge pharmacist, told Gaon Connection.
“When I am here, I attend to the patients but when I’m not here, the wardboy provides the regular medicines to the patients who have been coming to the centre previously. No new patients are looked after when I’m not here,” he added.

When asked about the situation at Pisawan’s PHC, Madhu Garola, CMO of Sitapur, told Gaon Connection that she will look into the matter. “Somebody else will be appointed to the health centre or the pharmacist will be sent back to the sub-center,” she said.
Also Read: Cancer survivor’s telemedicine centre links medics with villagers in remote areas
“It’s a difficult situation as the health department is understaffed as COVID19 has increased the workload of the doctors. I’ll look into the matter and check for how long this pharmacist has been doing his COVID duty,” she added.
Gaon Connection contacted Amit Mohan Prasad, Additional Health Secretary, Uttar Pradesh government for a response. But he was not available to comment. The story will be updated after his response is received.
Written by Pratyaksh Srivastava. With inputs from Sumit Yadav in Unnao, Mohit Shukla in Sitapur, Virendra Singh in Barabanki and Ramji Mishra in Shahjahanpur.

