Rural India reports 94% of snakebite deaths in the country yet primary health centres lack antivenoms, treatment facilities
Every year, 58,000 people in India die due to snakebites, with highest deaths in Uttar Pradesh (8,700). Even though antisnake venom is listed as an ‘essential’ drug for primary health centres, rural centres face an acute shortage of antivenom. Snakebite is among India’s most neglected public health crises.


Four species — cobra, Russell’s viper, krait and saw-scaled vipers — are the cause of 98 per cent of deaths in the country. Photo: Pixabay
Last August — August 3, to be precise — 23-year-old Sunita Meravi had a near death experience and it is a miracle, says Sunita, that she survived it. Sunita stepped out of her house in Katgo village of Kawardha district in Chhattisgarh and was bit by a snake. In no time, she turned pale, puked, lost consciousness and fainted.
And that is when the ordeal started. In an unconscious state, Sunita’s family rushed her to a health centre 15 kilometres away where she was given an injection and further referred to a hospital 120 kilometres away in Raipur, the state capital. It was a fight against time as her desperate family ran from pillar to post to save her life.
“We took her to the health centre on a scooter [two-wheeler]. She was given an injection but she was still unconscious. The centre referred her to Mekahara hospital in Raipur as that was the nearest hospital [120 kms away] with an ICU facility,” 28-year-old Shimla Meravi, Sunita’s sister, narrated the harrowing experience to Gaon Connection. “I thought we would lose Sunita, but she responded to treatment at the hospital and survived,” Shimla added.
The 23-year-old’s family managed to save her from becoming a part of India’s statistics on snake-bite deaths — an average of 58,000 deaths a year — which is almost half of the total annual snakebite deaths across the world.

A July 2020 study titled ‘Trends in snakebite mortality in India from 2000 to 2019 in a nationally representative mortality study’ shows that around 2.8 million cases of snakebites are reported every year in India; and in the past two decades more than 1.2 million have died of snakebites in the country. Up to 94 per cent of the snakebite deaths in the country are from rural India.
The July 2020 study also shows that 70 per cent of the snakebite deaths occurred in eight states — Bihar, Jharkhand, Madhya Pradesh, Odisha, Uttar Pradesh, Andhra Pradesh (which includes Telangana, a recently defined state), Rajasthan and Gujarat. Uttar Pradesh tops the list with 8,700 deaths a year followed by Andhra Pradesh (5,200) and Bihar (4,500).
Half of all snakebite deaths occur during the southwest monsoon seasons from June to September, when encounters between snakes and humans are more frequent at home and outdoors.
Map: Spatial distribution of snakebite mortality risk in India for 2004-13
Ironically, India is one of the leading producers of antivenoms but its rural health centres face an acute shortage of antivenoms, which is a leading cause of snakebite deaths, Kerala-based Jose Louies, who works with the Wildlife Trust of India, a non-profit conservation group, told Gaon Connection. “Snakebite is the neglected public health crisis in our country,” he added.
Delay in treatment
“Most of the snakebite deaths occur because of the delay in getting the anti-venom injection. Sometimes people resort to mumbo jumbo and witchcraft to treat the patient,” Shailendra Singh, Lucknow-based scientist from Turtle Survival Alliance that works on species that are at a high risk of extinction, told Gaon Connection.
Public health experts point out how most primary health centres (PHCs) at village level are ill-equipped to respond to snakebite cases. “Antivenoms are essential for the treatment. But, availability of antivenoms has always been an issue, especially in rural hospitals, PHCs, and CHCs, where it is most needed. There has always been a shortage,” Amulya Nidhi, a public health activist working on health rights in Madhya Pradesh, told Gaon Connection.
“The second aspect is the lack of ICUs [intensive care units]. Snakebites are not a priority for the government, because it is a rural-tribal centric illness, and not an urban issue,” Nidhi added. He is also a working member of the Jan Swastya Abhiyan, a national network of civil society organisations and people’s movements working for health rights.
This lack of access to antivenoms and delay in treatment was also highlighted in the July 2020 study, which said that most deaths and serious consequences from snakebite envenomation (exposure to venom toxins from the bite) are avoidable by timely access to safe and effective antivenoms.
Take the case of Sunita who had to be transported in an unconscious state over 120 kilometres away. “From the health centre, we booked a car and rushed to the hospital which was 120 kilometres away. Sunita regained consciousness only the next morning,” said Shimla Meravi, her sister. The family had to spend Rs 1,500 to reach the hospital, an amount that not many poor households can afford.
“I had lost hope that we would be able to save her. We were fortunate but not all tribal people here are,” Shimla added. According to her, snakebite cases were common in the villages. “Last year, fifty such cases from our village were reported, of which five people even died. They could not be treated in time. There are villages that are without electricity, water, and road connectivity,” she pointed out.
Also Read: Adivasis in India are being made to suffer a lot … and are being blamed for it too
The World Health Organization (WHO) also acknowledges that many people in India die of snakebites every year while on their way to a distant health facility.

“Most of the PHCs and CHCs do not have antivenoms. Sometimes people have to be taken to district hospitals which are generally twenty-thirty kilometres away from the villages,” Patna-based Shashi Yadav, president of ASHA Karyakarta Sangh, Bihar, told Gaon Connection. “Villagers are forced to visit private health centres or faith healers for treatment,” she added.
Anuj Kumar Chaudhary, medical officer, at a PHC in Fatehpur, Uttar Pradesh admitted lack of adequate health facilities. “Snakebites cases come here but we refer them to CHCs [community health centres]. They are given anti snake venom and tetanus injections. The antivenom is available only at the CHC level. The severity and time of treatment matters,” he told Gaon Connection.
Also Read: UP government makes claiming of compensation for snakebite simpler and quicker
Shortage of antivenom injections
There are about 300 species of snakes in India. Of these, only 15 are venomous. But only four of these 15 species — cobra, Russell’s viper, krait and saw-scaled vipers — are the cause of 98 per cent of deaths.
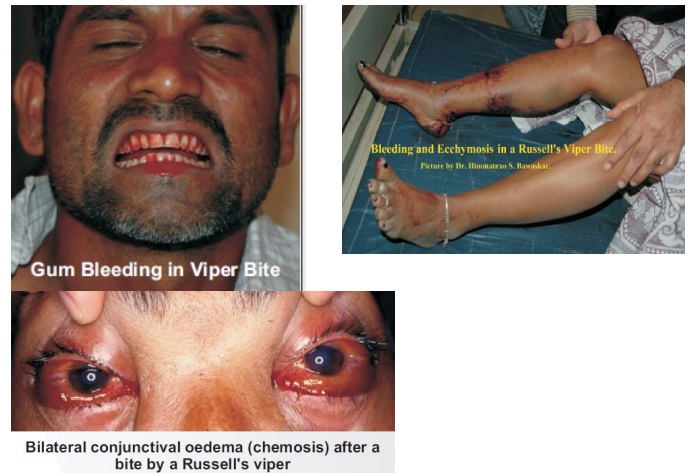
Bites by venomous snakes can cause paralysis that may prevent breathing, bleeding disorders that can lead to a fatal haemorrhage, irreversible kidney failure and tissue damage that can cause permanent disability and limb amputation.
Antivenoms are produced by injecting horses with venom so they generate antibodies against the toxins, informed Louies. According to him, the venom is collected only from Tamil Nadu and is used to manufacture antivenom to be used all across India.
Antisnake venom is listed as an ‘essential’ drug for primary health centres. According to the Indian Public Health Standard (IPHS) 2012 guidelines for PHCs, 24 hours emergency services include appropriate management of injuries and accident, first aid, stitching of wounds, incision and drainage of abscess, stabilisation of the condition of the patient before referral, dog bite/snake bite/scorpion bite cases, and other emergency conditions.
Quoting these guidelines, Nidhi said: “As per IPHS, all rural government hospitals including PHCs should have antivenoms. In flood prone areas [such as Bihar], the snakebite cases increase. Most of these cases happen during night time. It becomes very crucial to provide antivenoms on time. But the issue is neglected despite knowing its prevalence,” rued Nidhi.

“A large number of hospitals in rural areas lack antivenoms. But owing to the hospital apathy, many villagers are forced to move to private health centres where these antivenoms cost more than five hundred rupees,” said Jose Louies of Wildlife Trust of India.
“Every hospital at taluka level is supposed to have antivenoms. But many times, we see either these vials are not available or are old, meaning they have lost their efficacy,” Louies informed.
A Twitter thread by a physician based in Maharashtra, SP Kalantri, informed that antivenoms are often unavailable or unaffordable for the poor rural people, who are most likely to be bitten. “Most PHCs either do not stock enough antivenom or administer only a tenth of the full dose—a common practice,” he tweeted.
Dependence on quacks and local herbs
Predictably, with no access to adequate health facilities, villagers often end up visiting local jhola chaap (quacks) or traditional herbal practitioners for ‘all’ forms of snakebites. In the monsoon season, with highest snakebite cases, quacks do a brisk business.
“These days I do not have time to even have lunch. I will remain busy for the next three to four months,” Shobhan Singh Bisht, a traditional herbal practitioner, based in Thalisain village in Pauri Garhwal district of Uttarakhand told Gaon Connection. “People from many villages come to me. They come at any time of the day and night. I treat them using jadi buti [medicinal plants]. And in one or two days, they get cured,” he said confidently.
According to Bisht, who said he has been treating people with snakebites for over 30 years, there are no hospitals near hill villages for the treatment of snakebite patients. “People trust me with herbal medicines. If they do not get treatment for three hours, they die,” he said, adding that he earns Rs 50 to Rs 100 per patient.
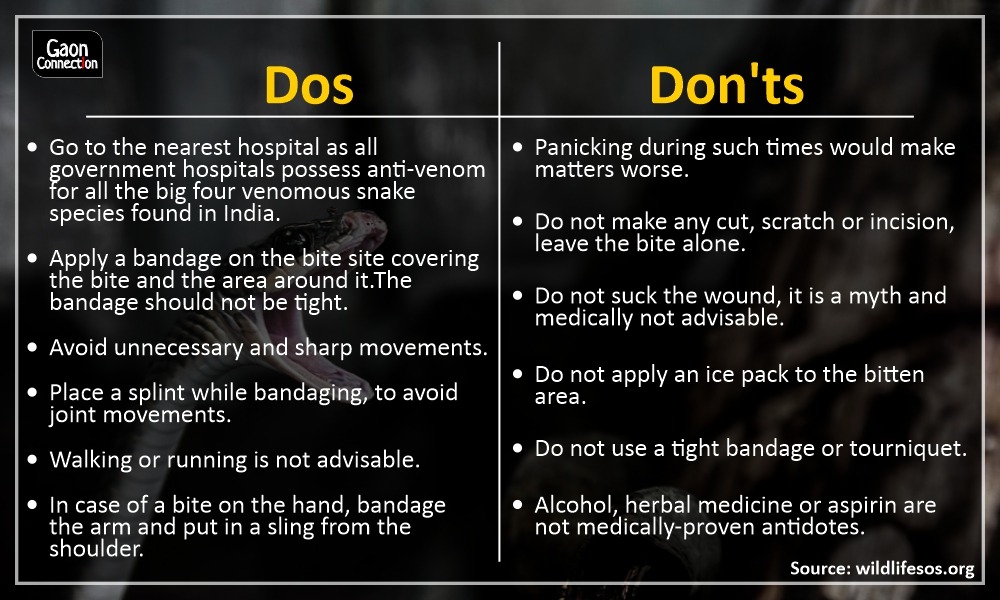
However, as per the WHO, traditional medicines and other treatments such as wound incision or excision, suction, or application of ‘black stones’ should be avoided in cases of snakebites.

Raising awareness and rescuing snakes
Despite India reporting the highest snakebite deaths in the world, there is a lack of awareness around symptoms and treatment for snakebites in its rural population.
“These snakebites are common in villages. Toilets are constructed a little far from home and often people encounter snakes,” Manjeet Kaur, a social worker associated with snake rescue operations in Raipur, Chhattisgarh, told Gaon Connection.
“Sometimes people do not even understand that they have been bitten by a snake. Only when the bitten part turns black, they understand it. If snakebite is reported on time, people can be saved,” said Kaur.
With the help of ‘We the People’, Kaur’s informal network of 50 volunteers, she has been involved in snake conservation and rescue operations since 1988.
“The snakebite cases generally increase in rainy seasons because places where snakes hide get flooded, for instance fields and rat holes. Food such as frogs are also easily available during monsoon,” she informed. “During monsoon, we get ten times more rescue calls,” she added.
According to her, awareness is needed at gram panchayat level. “Simple measures like taking torches at night can also prevent snakebites,” she said.
Experts suggest that wearing rubber boots and gloves while out in fields can help prevent snakebites. “They are a bit expensive [costing around Rs 500 a pair] for a villager but this can really be helpful. Often grains lying in the open attract rats thereby snakes. Ensuring cleanliness, proper lighting, avoiding dark corners, using torches while out can avoid such cases,” suggested Louies.
A non-profit Wildlife SOS suggests the following Dos and Don’ts for snakebites:
Serpent mobile app
While the rural health centres grapple with snakebite cases, a mobile application — Serpent — is coming to the rescue of rural Indians. Launched in 2016, this app includes a guide (at present only in English language) to all the snakes in India and a search facility to find the nearest hospital that treats snakebites.

The app can connect people with the nearest snake expert who can help them in a snakebite emergency. It also helps identify the venomous snakes by sending images to the experts. It also gives real-time reports about how many rescuers are out in the field, the number of snakes rescued and other critical data.
“A large number of households in villages these days have a smartphone. They know how to operate it. Taking this as an advantage, we developed an app that can help them find a nearest hospital that can treat snakebite cases,” Louies of Wildlife Trust of India, who helped launch the app, told Gaon Connection.
He added that “snake apps are like Ola and Uber for snake emergencies”.

