Testing Times: Screening, diagnosing and treating tuberculosis in 2020 took a backseat in India which has the world’s highest burden of TB cases
With all eyes on the COVID-19 pandemic, accessing health care for tuberculosis in the country became a serious struggle in 2020, as frontline health workers, healthcare centres and resources were deployed on COVID-19 duty.

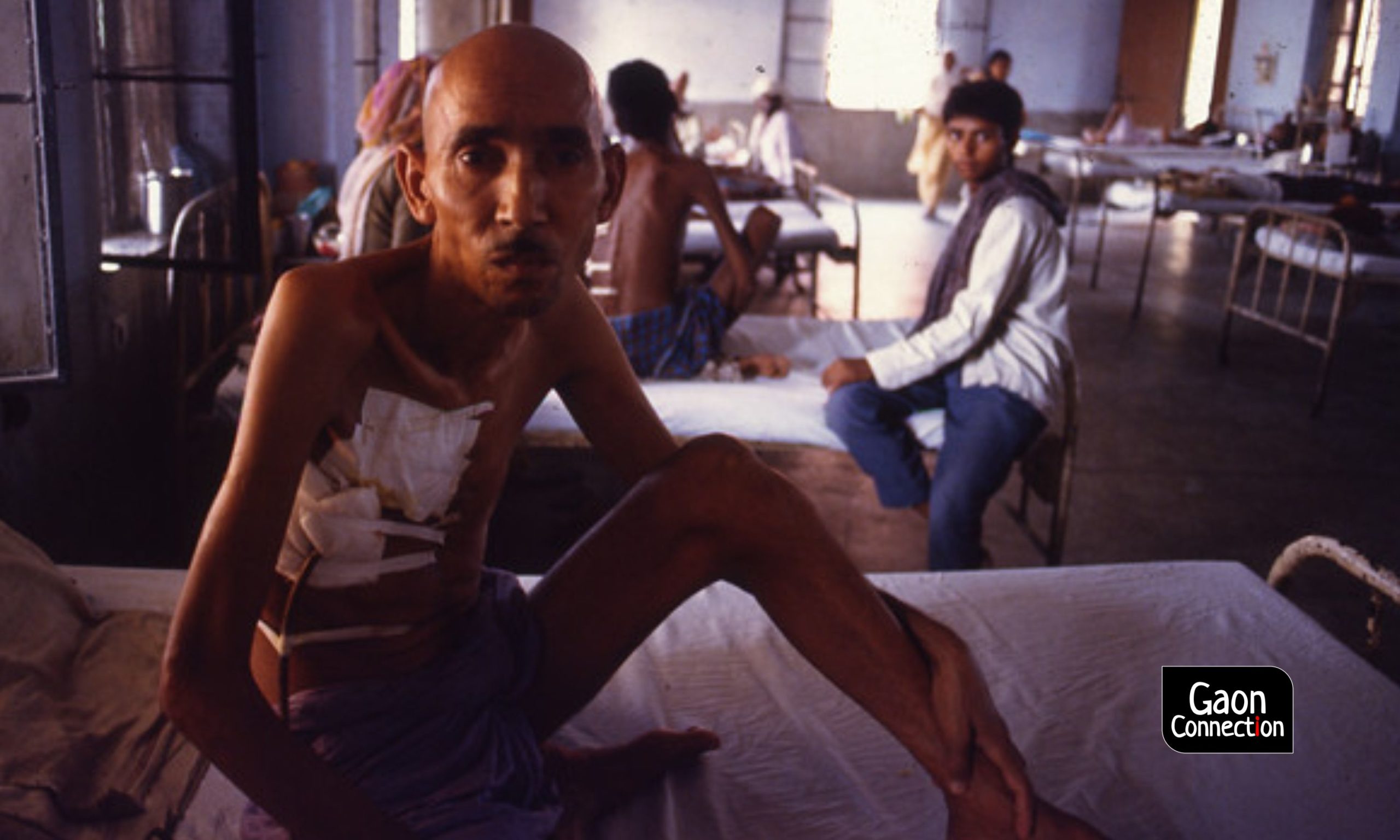
Tuberculosis patient in a healthcare facility in Delhi. Photo: Pradip Saha/flickr
Two years ago, 50-year-old Nimi Bibiyana Kujur of Ramgarh district, 46 kilometres from the state capital Ranchi, in Jharkhand, continued to receive drugs and treatment from the nearest health facility. But, the COVID-19 pandemic has thrown her treatment out of gear.
“With many healthcare facilities being converted into COVID-only ones, my mother’s treatment was stopped. She could no longer be admitted into the nearest health facility in case of any emergency,” Navin Kujur, her son, told Gaon Connection.
With an estimated 2.69 million new cases every year, India has the world’s highest burden of tuberculosis, according to the World Health Organization (WHO) report 2019. Every fourth Multi Drug Resistant-TB patient is from India.
“This year, because of COVID-19, TB care across the country has been affected. There were fewer and late diagnoses,” Sanjeev Nair, associate professor, department of pulmonary medicine, Government Medical College, Trivandrum, Kerala, told Gaon Connection.
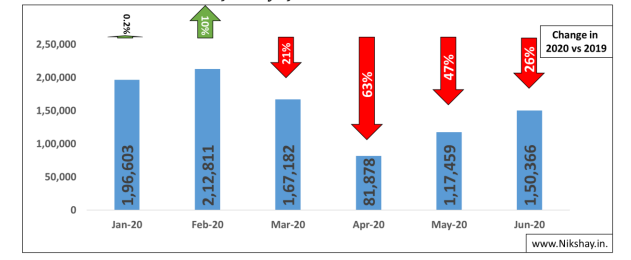
The COVID-19 led lockdown saw a major decline in TB case notifications, both in public and private health facilities. As per data from Nikshay portal, under the National Tuberculosis Elimination Programme, Ministry of Health and Family Welfare, overall, between March and June 2019, the public and private sector notified 860,787 tuberculosis cases in the country. However, last year, for the same time period, the public and private sector notified 465,051 TB cases. This is a drop of 46 per cent between 2019 and 2020.
“Screening, diagnosis and access to healthcare for TB patients were impacted in the last few months,” Anant Bhan, an independent researcher on bioethics, global health and health policy, told Gaon Connection.
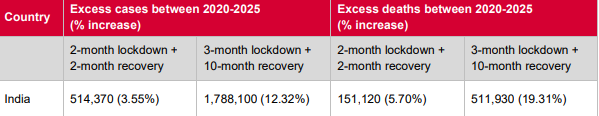
The writing is on the wall. As per the ‘Stop TB’ Partnership report published in May, 2020 as ‘The potential impact of the COVID-19 response on Tuberculosis in high-burden countries’, a two-month lockdown and a two-month recovery period for restoration of full TB services in India will result in an additional 5.1 lakh (0.51 million) TB cases and 1.5 lakh (0.15 million) TB-related deaths, between the years 2020 and 2025. With a three-month lockdown and ten-month recovery period, the numbers would be 17.8 lakh (1.78 million) and 5.1 lakh (0.51 million), respectively.
On September 25, 2019, Union minister for health and family Welfare Harsh Vardhan also launched the new TB Harega Desh Jeetega campaign as part of the government’s commitment to end-TB in the country by 2025.
However, it is estimated that the fight against TB faces a setback of five to eight years, globally, due to disruptions to health services, and delays in diagnosis and treatment caused by COVID-19.
Can we end TB by 2025
The Indian government launched the TB Free India campaign with the target of eliminating TB in the country by 2025, five years ahead of the global target of 2030.
The Indian government promises free diagnosis and treatment to all patients. In rural India, through Directly Observed Treatment Short-course (DOTS), a trained health care worker or other designated individual (excluding a family member) provides prescribed TB drugs and ensures the patient takes his or her medicines regularly.
In the month of April, last year, the Union ministry of health and family welfare directed states and union territories to ensure that the diagnosis and treatment of TB continue unhindered, despite COVID-19, and asked them to deliver a month’s dosage of TB drugs to patients.
“We have lost one complete year because of the pandemic. We will need a lot of patch up work to be done to bring our healthcare system to be fully functional for TB care,” said Nair, adding that the government would need more time to achieve its target to end TB by 2025.
So far, around 1.8 million people have died from COVID-19 worldwide in 2020. And almost 1.4 million deaths were recorded due to tuberculosis in 2019 alone across the world. Despite its widespread incidence, the services for tuberculosis, one of the oldest known diseases in the world, were ignored due to the pandemic.
For instance, 55-year-old Khumainyan Bai of Lamakheda village of Bhopal district, Madhya Pradesh, was diagnosed with tuberculosis in July last year, amid the pandemic. “We faced problems procuring medicines. We get medicines from ASHAs [Accredited Social Health Activist], but we had to go and collect medicines from them,” 35-year-old Santosh Ahirwad, Bai’s son told Gaon Connection. But, ASHA workers claim they are trying to do their best to provide care to TB patients.

Around one million ASHA workers have become the backbone of rural healthcare during this pandemic. They are the link between the health department and the villagers. But due to COVID-19, their services have been narrowed down to COVID-19 related duties, such as awareness campaigns on the coronavirus, door-to-door delivery of medicines, and surveying people in quarantine facilities.
According to the survey, The Impact of COVID-19 on the TB epidemic, more than 70 per cent of healthcare workers worldwide reported a decrease in the number of people coming to health facilities for TB testing. “In 2019, we had sixteen TB patients in and around four-five nearby villages. But last year, there were only four,” Parveen Bano, 41, who has been working as an ASHA for 12 years in Phanda block, Bhopal district, Madhya Pradesh, told Gaon Connection.
“We gave medicines to patients on time. Generally, all households take medicines and do not create a problem. But when they do, we make them take medicines in our presence, ” Bano reiterated. “Most of them try to hide the disease. But that is going to make things worse. We are expecting cases might increase next year,” feared Bano.
“Many symptoms of TB, for instance, a cough, are similar to that of COVID-19, and people are reluctant to get tested fearing that they will be taken away from their families and isolated for unspecified durations,” said Nair. This can exacerbate the problem, as undiagnosed patients can infect many more.
COVID-19 Vaccine and TB Vaccine
The ongoing pandemic also highlights the lack of attention towards diseases that existed before the novel coronavirus hit the globe. Commenting on the need for a new vaccine for TB, Bhan said: “Interest from both the public and private sector for a new TB vaccine is low. We need to do more research in that area. TB is a disease of poverty. It does not impact the rich and the middle class that much. But COVID does. Maybe, that is also why people are mostly focussing on the COVID vaccine.”

Resources for TB diverted for COVID response
As per the 2020 TB report, National Tuberculosis Elimination Programme, 1,180 CBNAAT (Cartridge-based nucleic acid amplification test to detect TB) facilities offer decentralised testing for TB at the district and sub-district levels.
“Machines used for TB diagnosis, such as CBNAAT, were also diverted for COVID-19 testing. Since testing was not available for many, diagnosis was affected,” pointed out Bhan.
“People who were not diagnosed earlier might have continued to spread it to others. Also, as people these days spend most of the time at home in close spaces, chances are they would have spread the disease to other family members,” he added.

Poverty and Poor nutrition
Undernutrition is a strong risk factor for developing TB and contributes to an estimated 55 per cent of annual TB incidence in India, according to the annual TB report 2020.
“One of the major factors for developing TB is malnutrition. But even if patients do not take nutritional support, they can cure the disease given they are diagnosed on time and take medicines properly,” said Nair.
Although, the Indian government has committed Rs 600 crore (six billion) for nutritional support of Rs 500 per month under the Nikshay Poshan Yojana to every TB patient through direct benefit transfer into their bank accounts, many like Bai haven’t received it. Her son Ahirwad said she received Rs 500 for nutritional support only once.
While the COVID-19 pandemic deserves attention and intervention, the response to it should not come at the cost of other health concerns. There has to be a lot more done if the country has to live up to the TB Harega Desh Jitega slogan.
Also Read: A disease that needs more attention than Coronavirus
Also Read: Tuberculosis and coronavirus: Challenges of managing an epidemic within a pandemic.

