COVID-19 has exposed India’s fragmented and disorganised blood transfusion system. It’s time to fix it
Despite the significance of blood, access to adequate, timely, and safe blood equitably across the country remains a health challenge in India. A hub-and-spoke model will enable smaller blood banks in rural areas to connect to a regional hub with advanced technologies.


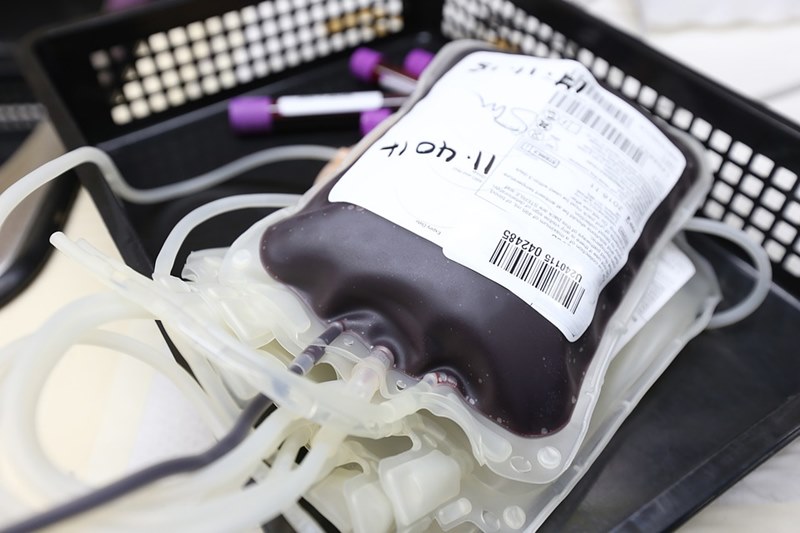
Access to blood is marred by misinformation and misconceptions around blood donation, especially in rural India. Photo: Pixabay
Saroj, a resident of Nagod, Madhya Pradesh, has a grim story to narrate about her visits to hospitals and blood banks in Satna district and other adjacent towns. Her father had multiple myeloma (a cancer of plasma cells) and needed transfusions twice a month. Every hospital or blood bank she went to urged her family and friends to donate blood in place of the units given to her father. For over eight months, she helplessly searched for donors until the last day of her father’s life.
Saroj’s experience is one that many patients and their families in India live through while in dire need of blood, and the situation only worsens in rural India.
With no WhatsApp broadcast groups for support, poor social media access to seek SOS help for blood, and no one to guide to the right resources, looking for blood for a loved one in rural India is heart-breaking and scary.
Despite its significance, equitable access to adequate, timely, and safe blood remains a massive public health challenge in India. As per the World Health Organization (WHO), at minimum, one per cent of the population must donate blood to meet a country’s basic blood requirement. In India, currently, only 0.84 per cent of the population donates blood voluntarily, leaving a shortage of over two million units of blood.
One of the most prevalent but preventable causes of maternal death is excessive blood loss after childbirth, technically known as postpartum hemorrhage. According to reports, about 30 per cent of maternal deaths in India are due to this excess blood loss. In rural India, several pregnant women (including high-risk ones) die because of delayed care and preparedness to handle risks associated with postpartum hemorrhage.
A fragmented, disorganised system
India’s blood transfusion system is fragmented and disorganised. Opening more blood banks is often hailed as a critical intervention to address the gaps in access to blood. However, the truth is that, with an acceptable blood bank density of 2.2 blood banks per million persons, India does not need more blood banks. It just requires more blood units and better coordination between blood banks to manage demand-supply gaps.
Also Read: In the middle of despair, CRPF Madadgaar is a ray of hope
Blood shortage also results from poor connectivity and communication among blood banks, which cause inefficient management of demand and supply both in terms of safety and availability of blood. Failure to properly process and store blood and its components separately leads to underutilisation and wastage of blood, more so in rural blood banks.
As part of its National Health Mission’s 2015-16 budget, the Government of India released Rs 20 crore to equip rural areas with blood collection and blood transportation vans. However, this initiative did not manage to meet its intended goal.
Meanwhile, inequities in access to and availability of blood have become particularly problematic due to the COVID-19 pandemic. The blood shortage crisis has only further compounded in rural and semi-urban areas. In the past several months, voluntary blood donations have drastically reduced due to the cancellation of mass blood drives and poor donor turnout owing to fears surrounding the coronavirus and resultant lockdowns.
Also Read: Meet constable Ashish Mishra who turned a messiah for patients needing blood

Misinformation around blood donation
Access to blood is marred by misinformation and misconceptions around blood donation, especially in rural India. People assume that donating blood will weaken their bodies or make them sick, and there is fear that the blood donation process is painful and could restrict their day-to-day functioning for a few days. Many women think they cannot donate blood, and several others believe they could contract infections, including HIV, from blood donation. The list of myths and ignorance about the effect and safety of blood donation is long.
As a result of inadequate voluntary blood donation, we see stories like that of Saroj emerging in villages, towns, and even cities, wherein blood banks and hospitals pressurise the patient’s families to replace the blood they used.
The low priority accorded to blood in the health agenda has translated into limited investments in blood transfusion infrastructure. This, coupled with limited voluntary blood donation, hugely impacts equitable access to blood in India.

Demand-led blood donation
Another big challenge in India is that the concept of blood donation is demand-led. In urban and rural settings, people donate blood in an emergency — when they are asked to or when there is a need in their own family and friends’ network.
Also Read: Meet constable Ashish Mishra who turned a messiah for patients needing blood
There is an urgent need for the country to build a sustainable voluntary blood donation programme in urban and rural areas. Through collective efforts of the government, civil society groups, community leaders, private companies, and media, it is vital to dispel myths and inculcate a cultural shift on blood donation as a social norm.
India’s blood transfusion system remains inaccessible and inefficient because it is not accorded the requisite priority in the country’s health agenda. There is a lack of coherence and commitment towards a focussed regulatory framework around blood safety and accessibility and investment in blood transfusion infrastructure.

Hub-and-spoke model
Therefore, it is crucial to think of a more effective and sustainable solution to the complex issue of improving the efficiencies of blood banks. There is merit in learning from successful models of blood transfusion systems worldwide to adopt an approach of partial centralisation of our transfusion system.
A hub-and-spoke model will enable smaller blood banks, especially in rural areas, to be connected to a regional hub with advanced technologies and a highly trained workforce to collect blood centrally and optimally process blood and its components.
After that, blood and its components can be transported to the various geographically dispersed storage centres or satellite blood banks located in rural areas to meet the local demand and needs.
With the support of a robust demand forecasting and inventory management system, this model can reduce blood wastage and ensure consistency in the safety and availability of blood and blood products even in the most far-flung places.
Also Read: Dialysis patients not getting consumables or easy access to hospitals during the lockdown
The COVID-19 pandemic has brought to the fore the fact that even when the healthcare capacity and focus shifts towards pandemic response, blood remains foundational to any healthcare system.
COVID-19 or not, can you ever imagine your body without blood? And so, as we reset and reboot our public health priorities in a post-pandemic world, it is vital to recognise the importance of blood adequacy, safety, and sustainability.
We cannot afford to have a myopic view towards the complex issue of blood shortage in India to imagine a country without avoidable deaths due to blood shortage.
Suryaprabha Sadasivan has close to 15 years of experience in policy research and advocacy. She leads the healthcare and social sector practice at Chase India, a leading policy research and advisory firm.
Views are personal.

