Hyper-local narratives are key to understanding the pandemic story in rural India
Despite sincere efforts to insulate them through check posts and quarantines, villages in India are not virus-proof. Migrant workers are not the sole reason for the spread of the infection in rural India.


The novel coronavirus came to India on international flights, initially affecting big cities like Mumbai and Delhi. More than six months into the pandemic, the virus is now gnawing its way across the country, though the recovery rate is almost 75%. Last week, India crossed the grim milestone of three million coronavirus cases. More than 57,000 people have already died. Many experts say these are conservative estimates; the real toll will be known much later.
How are the 600,000-odd villages in the country coping? To be honest, we don’t really know the exact extent to which the new virus has spread in rural India as yet because there is no authenticated disaggregated data. Numerous reports in recent weeks from across the country, however, suggest that India’s villages are not virus-proof, despite sincere efforts to insulate them through check posts and quarantines. Reasons for the spread of the infection in village India vary. They can’t be pinned down solely to the return of natives from big cities.
Hyper-local narratives about paddy fields, mandis and village roads are key to understanding what is happening on the ground.

Village markets and mandis are emerging as the new interfaces between the rural and urban population in some areas. Professor Sudhir Panwar of the University of Lucknow who has analysed data from rural and semi-urban areas of Shamli district in western Uttar Pradesh points out that in many parts of western UP, only a small population worked as labourers in Mumbai and other metropolitan cities. “In Shamli, most of those diagnosed with COVID19, were engaged in activities in the mandis, nursing homes and small shops. If migrant labourers were the sole reasons for the spread of the virus, then the ‘peak time’ for the spread of infection should have been April and May,” says Panwar.
Spread of infections in rural areas with weaker health infrastructure is hugely worrying. What is equally disturbing are attacks on frontline health workers — foot-soldiers in the COVID-19 detection efforts across India. Those engaged in swab collection, contact-tracing and referrals in rural areas are being abused and attacked, pointing to the challenges on the ground — fighting the virus and the attendant fear, stigma, and intimidation.
In recent weeks, a health worker has come under attack in a medical camp in Khanpur village in Punjab’s Ludhiana district when he was trying to motivate people with COVID19 symptoms to get tested. In rural areas of Jeypore in Odisha, frontline health workers engaged in swab collection are facing a difficult time trying to convince people to get themselves tested.

Media reports say local people are reluctant to give their swabs out of fear of testing positive and consequently, health teams are managing to achieve just about half of their swab test target. Last fortnight, a mob threw sticks and stones at a team of healthcare workers who were collecting swab samples for COVID-19 tests in Pagra Padri village of Uttar Pradesh’s Kush Nagar district. Vinod Sharma, a 40-year-old lab technician, was injured in the attack. The police have arrested five men who led the assault.
Such attacks can affect the fight against the virus. Errors by frontline health workers to trace people who have been in contact with infected individuals because people don’t speak out can put an entire community at risk.
What is fuelling the resistance towards frontline health workers? One big reason is fear of being confined and losing out on work in the time of acute economic distress.

“In rural India, there is no concept of ‘rest’ during the paddy season. People routinely go to work in the field even if they have slight fever. They don’t see it as a big deal. Their understanding of the virus is from lived experience, not from the big story about what is happening in the state or the country. Fear of death strikes only when someone in the village dies of the virus. People are worried that anyone suspected of having the coronavirus will be taken to the COVID Care Centre at the taluka level. and will be kept there for 14 days. They are afraid of being publicly identified as COVID positive and how it would affect their work. There is a belief that the virus is something that comes only from the ‘outside.’ ANMs travel to multiple villages on work. Unfortunately, in the prevailing atmosphere of fear and stigma, they have been targeted in some parts of India because they are seen as possible carrier of the virus,” Yogesh Kalkonde, a public health researcher and neurologist told Gaon Connection. Kalkonde is working with rural communities in Maharashtra’s Gadchiroli district.
Conversations with numerous ANMs (auxiliary nurse midwife) from across the country over the past week underscore the tremendous challenges frontline health workers are facing.
“It is a new virus. There is fear. People are afraid of social ostracization if there is a sign on their door saying they are COVID19 positive. They also worry about what would happen to their families, their livelihood. Sometimes, ANMs and other health workers who go on contact-tracing rounds are abused. But we carry on doing our work of awareness building, counselling, swab collection and so on, alongside all the other routine activities. There should be more recognition of our work,” Buluma Saikia, 51, Assam-based ANM told Gaon Connection. Saikia is president of the All India Federation of ANMs and LHV (Lady Health Visitors).
ANM Mamata Nayak from Khurdha, Odisha, who travels from village to village on a scooter also talks about the resistance people like her face sometimes while contact-tracing and referring cases to COVID Care Homes and fever clinics. Saikia and Naikia recently spoke at a online webinar organised by Women in Global Health, India – a first for both.

Can villages be hermetically sealed, realistically speaking? The answer is clearly ‘no.’
“In the time of the pandemic, many villages are trying to protect themselves by sealing themselves off. If you are coming into a village from the main road, you will be checked. But there are dirt tracks and village roads which are unmanned. It is impossible to monitor everyone who is coming in and going out. Local ASHA (accredited social health activist) workers are meant to monitor. They are doing their best but they are also from the village they work in, and are sometimes subject to pressure from local, influential people who may not want to report if they have symptoms suggestive of COVID19,” said Kalokonde.

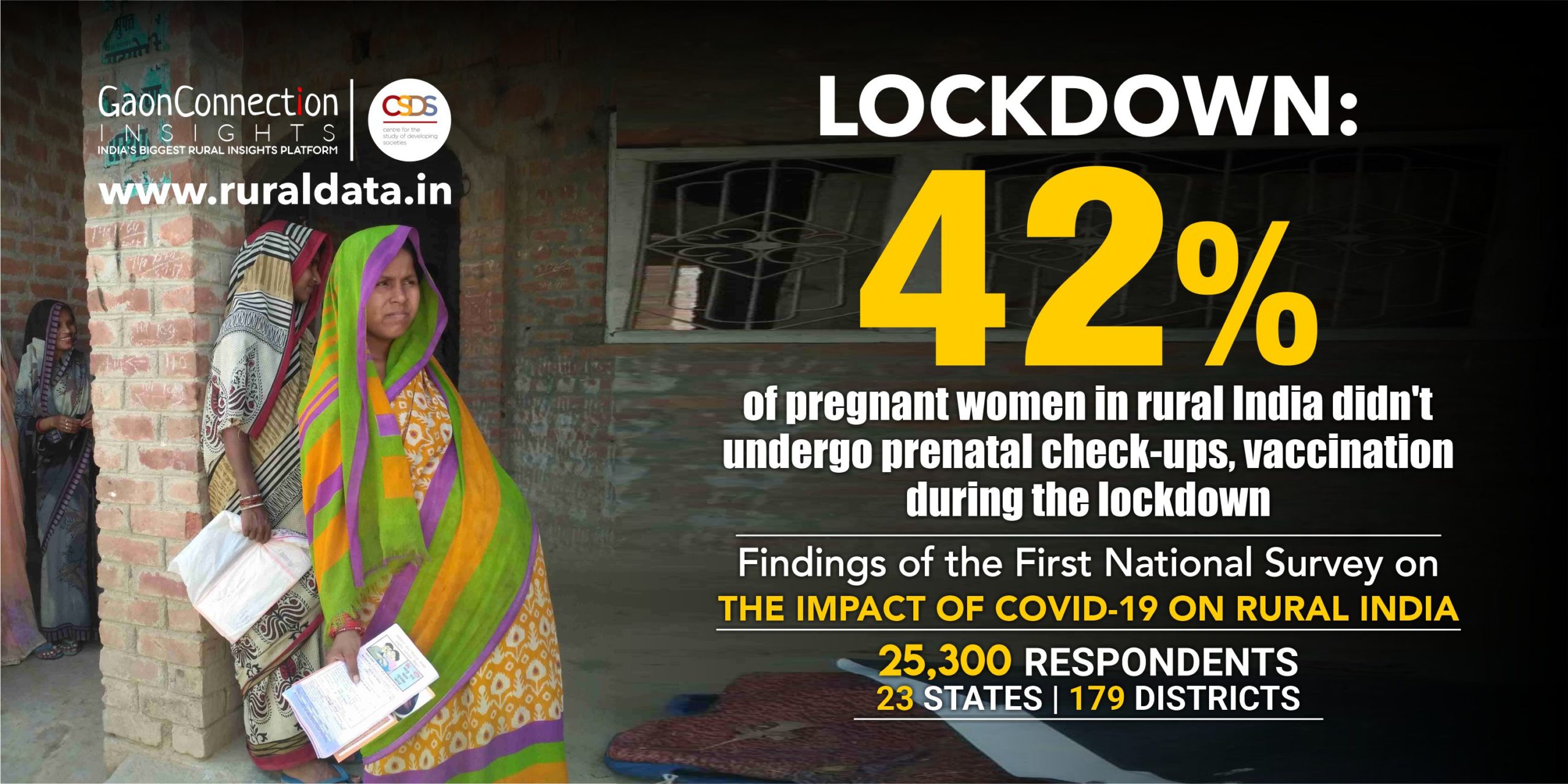
New data shows these challenges come on top of old ones in rural India. A recent national survey on the impact of COVID-19 lockdown on rural India by Gaon Connection and New Delhi-based Centre for Study of Developing Societies, reveals mounting debt, increasing hunger, complete loss of livelihoods, and inability to access healthcare.
The survey, the first-of-its-kind, based on face-to-face interviews with 25,300 respondents in 179 districts across 20 states and three Union Territories by Gaon Connection Insights, the data and insights arm of India’s largest rural media platform, shows that around one in every eight households in the survey (11%) reported having a pregnant woman in the household, and nearly three fifths such households (58%) confirmed that pre-natal checking and vaccination had happened in their village. The findings throw up a mixed picture. Clearly, while many pregnant women were not denied the medically necessary care they needed, many (42%) seem to have had to go without it.
The virus of stigma in the time of the pandemic is not unique to India. “Amid growing mistrust, health care providers increasingly come to be seen as a risk to communities rather than the solution to this public health emergency,” said the World Health Organization.
How we communicate messages about COVID-19 in villages is going to be critical in how the virus pans out in rural India. As Kalkonde puts it “A lot will depend on village leadership and local de-stigmatisation campaigns.”

